Author’s Corner
In this white paper, Silas Goldman, AVP of Operations, reviews the common attributes of successful population health management and reveals how they can be achieved. Silas also covers prognostics and health management strategy, including digital adoption, disease identification, clinical intervention, and patient engagement.
Watch the video on the right to learn more about Silas, his paper’s key takeaways, and his motivation for writing on this topic.
To discuss this white paper in more detail, please contact the author using the information provided at the bottom of the page.
The year 2020 offered the difficult realization that the lack of sufficient public health data systemically hindered the U.S. healthcare infrastructure’s ability to timely fight a pandemic.
The systemic impact of COVID-19 garnered headlines across the globe; however, those living in the value-based care industry who focus on SDoH and chronic disease management are all too familiar with leveraging health data to predict and prevent acute illness events.
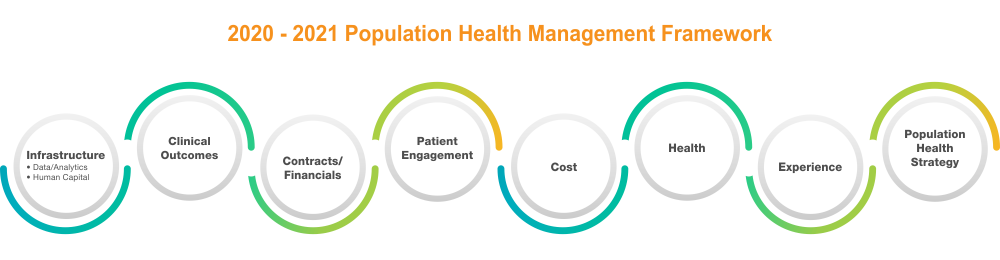
High performing healthcare entities integrate a combination of analytics, clinical care coordination, and patient/member engagement to define their internal population health management solution. Common attributes associated with successful population health management strategies include:
- Early identification and stratification of at-risk (potentially liable for increased severity of illness) populations
- Early interventions using a hybrid Machine Learning (ML) and human capital expertise
- Cohesive partnership with patient and provider to manage overall health
Early adopters of population health management endured a significant learning curve since PPACA with regard to investing in ML/AI tech against an expected ROI. Vee Healthtek has observed consistent improvement across payers and providers to leverage digital population health management tools to meet fiscal and value-based targets.
The New New
Claims data remains the backbone for most digitally connected population health suppliers and users, which also makes users vulnerable to time/accuracy issues with any claims-based solution. For the time being, disease identification, stratification, and clinical intervention will remain a hybrid use of tech for clinical data integration augmented with professional services.
At Vee Healthtek, our clients strongly support pursuing “technology-enabled” services where our critical differentiator is the ability to avoid being fully contingent on data or human capital.
The fluid revenue stream associated with value-based care will keep population health management in the “maturing technology” category. The purpose and principles of PHM intersect with broader industry dynamics, particularly digital evolution. Eventually, the value-based sector will separate, leaving those who adopted a digitally connected population health strategy well positioned to navigate the increase in M&A activity versus niche entities that may be non-scalable in the new new.
2021 Reality
In 2020, healthcare entities were scattered across all levels of population health maturity, strategy, adoption, and digital integration to support an integrated care model. In the payer sector, several regionalized markets of the Big 5 (UHC - 70 million, Anthem - 40 million, Aetna - 22.1 million, Cigna - 20.4 million, Humana - 16.6 million2) saw the fruits of their PHM strategy align with the incentive and revenue models.
Our recommendation for 2021 is to define the transformation roadmap for integrating a PHM strategy, which includes digital adoption, disease identification, clinical intervention, and patient engagement.
References:
2 https://www.beckersasc.com/asc-news/5-largest-health-insurance-companies-by-membership.html

