A true 360-degree understanding of all parties within the healthcare ecosystem isn’t just to be preferred, it is absolutely a prerequisite to a thriving business
The traditional understanding of the delicate ecosystem among the three critical players in the insurance industry are:
When a TPA is involved, #3 is not the payor directly, but rather the TPA firm hired to handle the plan and claims between the employer/plan/patient and the medical provider.
This paper examines the business challenges, solutions, and outcomes when Vee Healthtek was called upon to take over nearly all claims-related, call-related, and billing-related third-party administrator services for a leading TPA in the Midwest that deploys solutions for employers, professional employer groups (PEOs), associations, brokers, and healthcare providers.

Our client had some serious problems in 2013
- Turnaround time on repricing and adjudicating client claims was lagging
- Quality employees were hard to come by in their region
- Volumes were difficult to predict due to seasonality and a cyclical 'busy season' from November to February that decimated planning, resourcing, and other considerations from a volatility perspective
The client needed a variable approach to fixed problems. They needed high quality talent… rapidly. Nearly all their processes had become highly customized over years of tweaking; their primary electronic system was homegrown and nuanced.
Finding a vendor was necessary, but finding the right partner was critical. Time was also of the essence, as claims were backing up daily.
Vee Healthtek's Solution
The TPA turned to Vee Healthtek for help on all fronts.
In 2014, Vee Healthtek put into place single points of contact, communication channels, weekly processes, and frequently visited client sites to build intimacy. Creating this basic framework gave them and us a platform to measure accuracies, validate competencies, and begin the slow process of building teamwork.
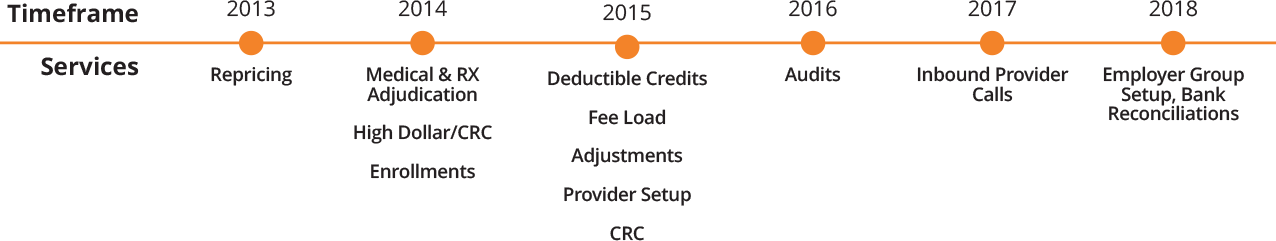
Together, the TPA and Vee Healthtek have expanded services to over 13 different claims-related, call-related, and billing-related functions. Business has grown year over year since starting the relationship nearly six years ago – helping the company hit record results, increase revenue upwards of 45%, and set up incredible future growth.
Vee Healthtek could not have taken over 13 different services, across 3 business verticals, if it was not for the positioning of key personnel at the top, from the start.
The General Manager of Claims Services at Vee Healthtek managed the due diligence, implementation, ramp up, governance, and review of all services from day one. He has been with Vee Healthtek since its first payor client, building experience installing a myriad of TPA-related services over a 20-year career.
He states that the key to building out a successful account management model for a TPA is “studying the interoperability of all the different tasks a TPA takes on and building a specifically trained team that can achieve those outcomes across the departments that drive daily activity.”

Conclusion
While Vee Healthtek took on only two service lines in the beginning, it positioned itself to handle all of its client’s challenges, collectively, from the start – whether directly involved or not. This "eye level" approach is the only way to properly prioritize client needs, contextualize demands, and build a sustainable partnership predicated on achieving long-term outcomes.
As the client's Chief Operating Officer remarked last year, "Nearly three years ago, I was looking for cost-effective and high-quality claims processing support services. We were looking to supplant our internal teams with bandwidth. Vee Healthtek quickly set up training, account management, sourced resources, and built processes with my team. Additionally, we have expanded our relationship with them over the last several years. While we originally sourced claims re-pricing and adjudication support services, we have now expanded to have Vee Healthtek do our enrollments, reenrollments, adjustments, null/voids, benefit setup, and high dollar claims. We are additionally exploring having Vee Healthtek take over several claim audit functions as well."
