Payer prior authorizations are expensive and administratively daunting. A high failure rate lowers care outcomes and drains revenue. However, we’ve found that process discipline and automation unshackles clinical staff, with big boosts to care quality and revenue.
Unseen Consequences
Payers require authorization prior to many procedures and for specialty drugs to assure medical necessity and effectiveness. This enables patients to receive appropriate care while reducing waste. However, it’s not clear that prior authorizations actually reduce costs. One study found 24% higher plan-paid costs for members requesting a Type 2 Diabetes medication requiring prior authorization (PA) but not receiving it, compared with those who qualified for and received the requested medication. [1]
Dysfunctional prior authorization (PA) processes drive up costs and reduce patient access to care. Physicians report that engagement with payers on medical necessity and PAs results in:
- High administrative costs – Nearly $94,000 per year per physician [2]
- Abandoned treatment – One study cited 40% of patients confronted with a prior auth requirement just didn’t pursue it any further. [3] And 92% of doctors say prior authorizations have a negative impact on patient clinical outcome. [4]
- Uncompensated care – The source of 74% of physician write offs. [5]
Clinical and office staff must navigate unique processes for each payer, plan, employer, procedure, and medication. Requirements change frequently with unclear standards. No help comes from technology as only 12% of transactions nationwide have been automated––and only the very simplest. [6] Denied claims sit unworked since they’re the most difficult and time-consuming task.
Not obtaining a proper PA drastically impacts practice income. Plans refuse to pay and preclude direct billing of the patient. Satisfaction of both the patient and provider suffer. No wonder most primary care providers see the prior authorization process as unsustainable.
Get the Process Right
For our clients, we utilize our RevAmp platform to create efficiency by mapping processes in detail and automating the parts not requiring expert judgement. We start with a tangled mess, move toward discovery of critical knowledge, and organize it for reuse and visibility.
When a physician orders a procedure, test, or medication, we proceed through payer-imposed process steps:
- Check rules – Map the patient’s health plan PA rules on website or by phone.
- Obtain forms – Determine and retrieve the documentation requirements.
- Gather documentation – Use the physician order and existing EHR documentation to satisfy PA rules.
- Submit documentation – Complete and assemble the payer’s form and attach required documentation. Fax or upload the package.
- Monitor process – Dog the plan for approval or rejection. Follow up by voice when timing of care is critical.
- Feed the EHR –Extract documentation from payer website when approved and update EHR screens for clinical, HIM, billing, and compliance documentation.
- Handle rejection – Determine additional documentation requirements. If needed, query the physician’s staff.
- Peer review (if documentation requirements cannot be satisfied). Schedule a peer review for the RN or physician with the Plan’s clinical staff. We drive these events below 5% of PAs.
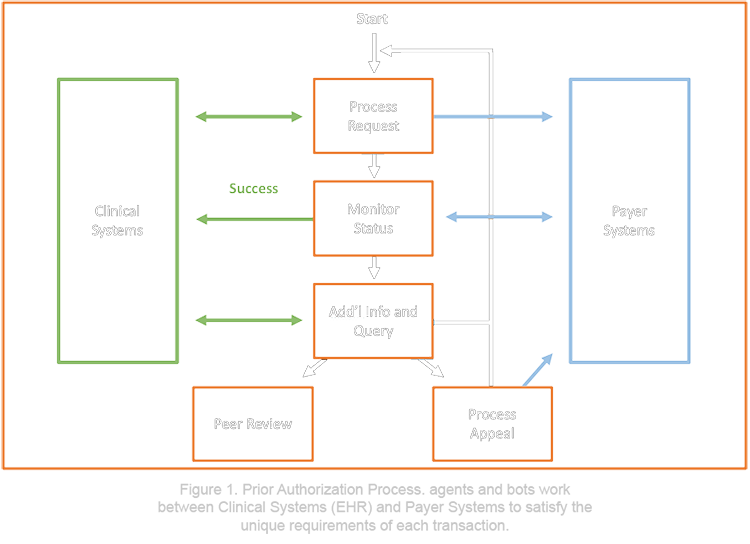
Our agents execute repeatable but often complex scenarios between inherently incompatible systems to drive each transaction for approval. We start completely manually then enable “bots” to work alongside agents.
Unfortunately, each step can get off track with a new rule, a gap in documentation, a moment’s inattention, or system errors. The whole process varies by payer, plan, procedure, test, medication, employer, individual patients, and even each iteration. It’s breathtakingly tedious. Still, we work backwards from a goal of first-pass success with continuous improvement.
Automation Relief
To create a solution space for automation, we scour processes for repeatability. When every process varies every time, that’s tough. We handle complexity by building “scenarios” shared between agents and bots. Business analysts find the tall Pareto bars of repeatability and dig in to definitively describe each series of transaction segments and source data to automate them.
Our usual suspects for repeatable automation of any clinical system or payer system transaction include:
- Extract transaction rules and forms from payer website
- Access patient information in EHR
- Fill forms
- Extract clinical documentation from EHR
- Upload or fax documentation
- Record action logs
- Monitor and inquire for status
- Download approval documentation from payer website
- Populate multiple EHR screens to enable downstream processes
We differentiate between the highly repeatable process segments and the steps where control must be handed back to the agent for quality checks and complex assessments. In the case of PAs, we build dozens, sometimes hundreds, of scenarios within our RevAmp workflow automation platform. Each leverages a common process framework but adjusts to nuances of payer, plan, procedure, test, and medication.
After investing twice as much business analysis compared with the actual automation, our robotic process automation (RPA) engineers can pull out their tools. They build reusable modules for pulling and pushing information from the EHR and the many payer websites. They can then assemble scenarios to execute automatically through repeatable parts and return control to an agent for hard parts.
In production, our agents focus on the barriers to success by making critical decisions. Our Robotic Process Automation then executes repetitive actions for them across disparate systems that vary across patients, while they sort out one-off problems.
Astonishing Outcomes
From the starting point of a dysfunctional prior authorization process, our discipline and technology integration experience drives winning outcomes for the patient, the clinical staff, and the practice:
- Reduce time to completion – Patients get care quickly
- Reduce clinical staff time significantly – Available for patient care
- Reduce physician attention – Only involved in the rare situation requiring peer review
- Reduce denials – Eliminate high occurrence of refusal to pay
- Reduce AR backlog – Accelerate cash through higher first pass success
- Deliver higher revenue – Reimbursed for services provided
Using process engineering discipline, scenario-guided agents and Robotic Process Automation development, we’ve unshackled clinical staff with big boosts to care quality and revenue.
References:
1. J. G. Bergeson, et al. (2013). Retrospective Database Analysis of the Impact of Prior Authorization for Type 2 Diabetes Medications on Health Care Costs in a Medicare Advantage Prescription Drug Plan Population. JMCP
2. L. P. Casalino, et al. (2009). What Does It Cost Physician Practices To Interact With Health Insurance Plans? (in 2020 USD). healthaffairs.com
3. D. Rubin, (2017), Tackling the Prior Authorization Challenge: A Critical Task for Pharma. pharmaexec.com
4. 2017 AMA Prior Authorization Physician Survey. AMA
5. (2018). The Shocking Truth about Prior Authorization Process in Healthcare. getreferralmd.com
6. CAQH Explorations. 2018 CAQH Index. A Report of Healthcare Industry Adoption of Electronic Business Transactions and Cost Savings. caqh.org
