We joined healthcare finance leaders at the Healthleaders Revenue Cycle Exchange in Sarasota, Florida. The audience? Health System CFOs. Chief Revenue Officers. Senior Vice Presidents of Revenue Cycle. The agenda? Healthcare Revenue Cycle Management (RCM) under pressure - operationally stretched, financially scrutinized, technologically saturated.
Cautiously ambitious.
Pragmatically innovative.
Below are the architectural themes that stood out - and what they mean for modern Healthcare Revenue Cycle Management.
AI Is Here - But It’s Task-Optimizing, Not Headcount-Reducing
Nine of the thirteen sponsors at the event were AI-first technology firms. If momentum were measurable by conversation volume alone, automation would have dominated the agenda. But inside the roundtables, the tone was different. AI is not replacing revenue cycle teams. It is redistributing effort.
AI is creating capacity, not reducing headcount
The highest ROI use cases discussed were precise, contained, and measurable:
- Payer policy scraping bots saving ~40 hours per month
- Underpayment recovery teams generating 20:1 ROI
- CDI prioritization engines guiding reviewers to likely documentation gaps
- Predictive analytics identifying denial drivers before submission
The lesson? Blueprint before build.
AI succeeds when applied to repeatable tasks with clear ownership and measurable outcomes. End-to-end “revenue cycle transformation by switch activation” remains fiction.
Denials Are Rising - The Real Work Is Upstream
Denial rates across systems hovered between 10–15%, with struggling organizations pushing toward 20% and above. The most concerning trend? Clinical denials. Documentation gaps. Medical necessity. Missing elements that originate not in the billing office - but in the clinical encounter.
We don’t have a denial problem. We have a documentation discipline problem.
The shift underway is from reactive appeals to predictive prevention:
- Root cause identification by payer, procedure, and diagnosis
- Accountability for denial drivers within operational teams
- CDI embedded earlier in workflow
- AI surfacing likely denial triggers before submission
This is not about writing better appeal letters. It is about engineering fewer denials into existence. Prevention is cheaper than persuasion.
Enterprise EHR Platforms are the Foundation - But Not the Entire Structure
Every large system represented operates an EHR Platform. Yet a striking theme emerged: Turning functionality “on” is easy. Operationalizing it is hard.
Leaders were candid:
- EHR automation still requires human oversight
- Enablement demands IT staffing, training, certifications, and ongoing investment
- Some AI capabilities within EHR remain maturing
The strategic debate wasn’t one platform versus another. It was this: “What is the true 20-year cost of internal enablement versus outcome-based partnerships?”
Modern RCM is not a single-platform play. It is orchestration - specialized tools across front, middle and back office. One system of record, multiple systems of optimization.
Vendor Expectations Have Changed - Permanently
If there was one unmistakable shift over the past decade, it is this: Health systems will not subsidize vendor learning curves.
We can’t pay you to figure us out.
Expectations now include:
- Conservative ROI modeling
- Shared accountability
- Performance-based contracts
- Defined SLAs tied to denial reduction, A/R improvement, productivity
- Real-time operational visibility
Partnership is no longer a slogan. It is a risk-sharing structure. Trust is not earned by capability decks. It is earned by measurable outcomes.
Workforce Reality - Automation Changes Roles, Not Necessarily Headcount
There was a contrarian tension throughout the event: AI investment is accelerating. Labor shortages persist. Why? Because most health systems are not overstaffed. They are understaffed.
The focus is shifting toward:
- Repurposing talent
- Upskilling adaptable performers
- Identifying “diamonds in the rough”
- Paying for skill without forcing management promotion
I don’t have people. I have a person
Small and rural hospitals face amplified constraints - limited staff, older platforms, cultural barriers to collections. For them, automation is less about transformation and more about tool augmentation. Technology must reduce friction, not remove humanity.
Evolution Beats Revolution
One misconception quietly dissolved during the discussions: Massive platform change is not the primary differentiator of high-performing systems.
The leaders are winning through:
- Workflow restructuring
- Operational accountability
- Real-time performance visibility
- Process discipline
More evolutionary than revolutionary. More engineering than theater. Modern Healthcare Revenue Cycle Management is less about buying something new - and more about architecting what already exists into a cohesive system.
The Quote That Stayed With Us
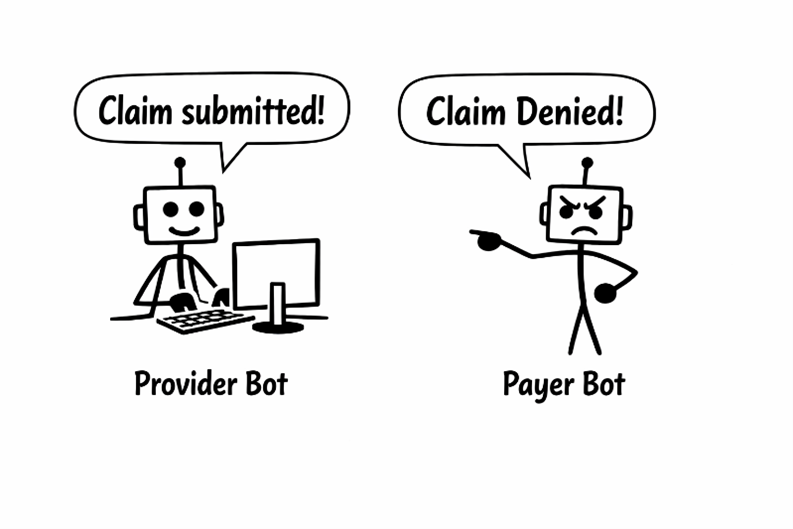
One session described the emerging landscape as: “The battle of the bots.” Hospitals deploy bots to submit cleaner claims. Payers deploy bots to review, delay, or deny. Automation versus automation.
Which means the future of RCM is not simply digitized workflows - it is strategic counter-automation. The systems that will thrive are not those with the most bots.
They are the ones with:
- Clear use-case discipline
- Structured ownership
- Transparent ROI
- Operational readiness
Automation without architecture becomes noise.
What CFOs and RCM Leaders Should Prioritize Now
From dozens of conversations, three leadership imperatives emerged:
- Build a Task-Based Automation Roadmap. Not a technology roadmap. Define the task, quantify the pain, then deploy precision tools
- Engineer Denial Prevention Upstream. CDI, documentation feedback loops, predictive analytics - prevention is margin protection.
- Demand Measurable Partnership. Outcome-based contracts. Transparent SLAs. Shared accountability.
Revenue cycle is no longer a back-office function. It is financial infrastructure.
Final Reflection - Resilient Systems Win
The real takeaway from the event was strategic clarity. Healthcare Revenue Cycle Management is entering a phase of disciplined modernization: Innovative, but pragmatic. Ambitious, but accountable. Technology-led, but human-aware.
And that, more than any bot, will determine who wins the next chapter of revenue cycle.



