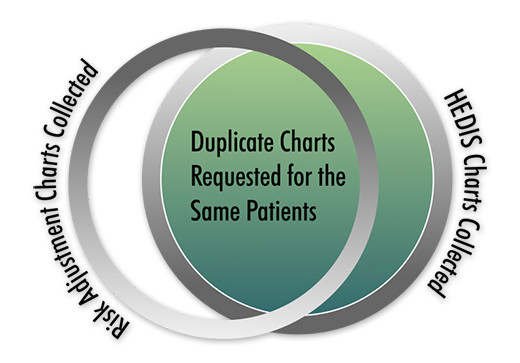
Although health plans annually perform both Risk Adjustment reviews and HEDIS quality abstractions, there is significant duplication of efforts when obtaining the charts needed for both programs because there is often little communication between them. Imagine the frustration at a provider’s office while they fax the same records to the same health plan, but to two different fax numbers.
A recent conversation with a Vee Healthtek client revealed his frustration after learning the two departments, Risk Adjustment and Quality Metrics (HEDIS), had requested, received, and uploaded nearly 60% of the charts from the same providers for the same patients. Once would have been sufficient. Unfortunately, these charts were in separate databases not shared between the two departments. And since no sharing occurred, there sat nearly 10,000 duplicate records.
This is obviously not an efficient use of healthcare dollars. A solution to the problem could provide a 60% savings in time and money to Vee Healthtek clients.
First, a brief review of the two departments involved:
- Risk Adjustment – It provides chart reviews for coding accuracy and allows health plans to capture funds they may not have received based on the acuity of their patient population. Health plans voluntarily participate in these reviews.
- Quality Metrics - HEDIS (Health Effectiveness Data Information Set) It provides HEDIS data collection used to calculate a Star Rating for the health plan. 1-Star is the worst and 5-Star is the best. Health care plans, required to participate, receive bonuses and rebates based on their Star Rating. HEDIS is owned by the National Committee on Quality Assurance NCQA.
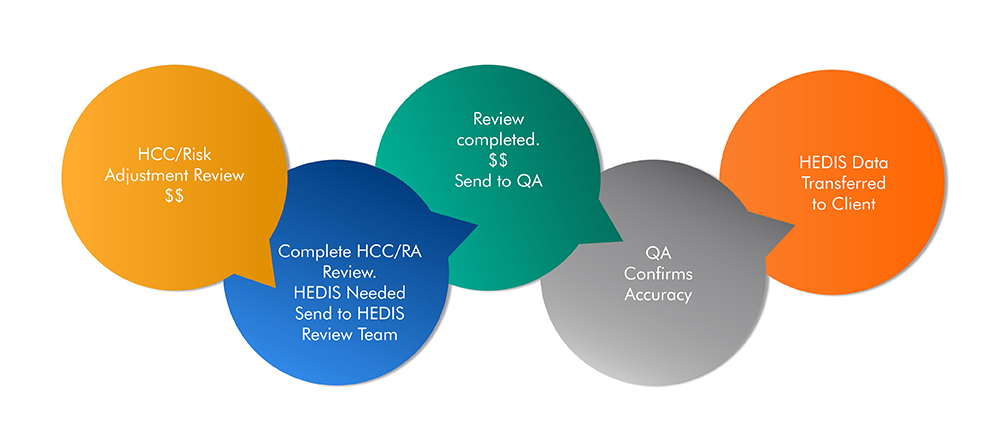
Vee Healthtek understands the value of offering a bridge between these two departments to its clients by combining Risk Adjustment reviews and HEDIS data collection.
Benefits
- Eliminating duplication of efforts between Risk Adjustment and Quality (HEDIS) departments
- Reducing provider abrasion by minimalizing duplicate chart requests
- Saving money and manhours by reducing the overall number of chart requests
- Giving the appearance of being a more cohesive organization
- Providing a year-round project for clinicians and certified coders
Concerns with this model to consider:
- Would it cost additional money to gather HEDIS year-round and during HEDIS season?
Answer: No - The same number of HEDIS measures will be collected annually whether collected year-round or during HEDIS season.
- Will HEDIS data be collected that isn’t needed by the health plan?
Answer: No - Health plans generate reports of missing HEDIS data regularly to share with their providers. With access to these reports, only data needed would be captured.
- Where will data be stored until ready to upload for HEDIS season?
Answer: Not determined. This will require a review of the health plan’s software capabilities or perhaps research into a third-party software program.
- Will we need to employ twice as many people to cover both Risk Adjustment and HEDIS reviews?
Answer: Vee Healthtek has skilled clinicians and certified coders capable of performing both reviews with proper training. Staff would have to be adjusted based on the increase in volume of reviews.
Vee Healthtek currently offers both Risk Adjustment reviews and HEDIS abstractions as one of its many services. Creating a workflow incorporating a seamless transition from Risk Adjustment reviews to HEDIS data collection can be invaluable to organizations.
