Author’s Corner
In his white paper, Mark Kausel, Senior Director of Client Success, provides insight into accountable care organizations (ACOs). Specifically, Mark covers ACOs’ need for an inclusive and collaborative culture that involves everyone in the organization.
Please click on the video to the right to learn more about the author, his paper’s key takeaways, and his motivation for writing on this subject.
To discuss ACOs at length, please contact Mark using his information provided at the bottom of the white paper.
The Affordable Care Act prompted many innovative care delivery and payment reform initiatives to address both the daunting growth of healthcare costs and less than optimal patient care outcomes. One of those unique initiatives was the accountable care organization (ACO).
The mission for all ACOs is to deliver high-quality care for lower costs, which is done by effectively managing gaps in quality and risk. Through this model, physicians, hospitals, and other care providers deliver coordinated, high-quality care to their patients.
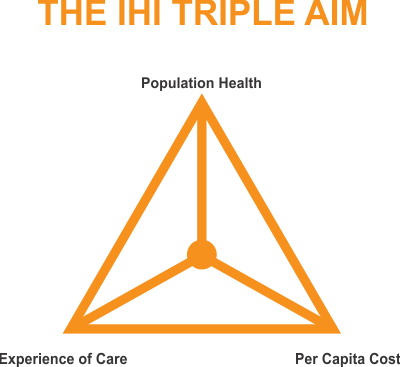
These organizations achieve these goals using a universal budgeting system and value-based reimbursement. The framework for the design of ACOs can be found in the model introduced by the Institute for Healthcare Improvement (IHI) known as the Triple Aim for Populations.
According to the IHI, “successful health and health systems of the future will be those that can simultaneously deliver excellent quality of care, at optimized costs, while improving the health of their population.”
Delivering Quality and Mitigating Risk
There is no mandated standard for ACOs. Each organization operates with different funding structures, metrics they report on, and payment agreements that vary from group to group. Some include specialists and hospitals, while others focus on providing primary care services. The populations they care for all have unique characteristics and needs, so funding is impacted in two ways – quality scores and a risk adjustment factor score.
For the 2020 and 2021 performance years, the Centers for Medicare & Medicaid Services (CMS) has provided twenty-three (23) quality performance benchmarks for ACOs participating in the Medicare Shared Savings Program (MSSP). They are categorized into four quality domains – Patient/Caregiver Experience, Care Coordination/Patient Safety, Preventive Health, and At-Risk Population.
A key measure of success for all ACOs is to improve these quality scores, centered around delivering high-quality patient care. It is important to be able to identify gaps in care and enable care providers to address them and document appropriately. ACOs monitor the gaps in care for their members, and based on how well these gaps are filled, providers can earn shared savings payments.
Risk Adjustment Factor (RAF) scores are used by CMS to estimate probable costs for Medicare Advantage beneficiaries and are derived from Hierarchical Condition Categories (HCC) along with demographic factors. HCCs are based on ICD codes identified from claims data and retrospective reviews of encounter documentation. These reviews often identify gaps in care that were not identified and documented appropriately by a provider and can have financial implications. As an example, a review completed on a 76-year old female increased the patient’s HCC RAF score from 1.029 to 3.633. This increased the annual member payment by $21,000.
These gaps in care can have a significant impact on quality performance scores and Risk Adjustment Factor scores, and ultimately a providers’ reimbursement. It is critical for ACOs to identify and eliminate these gaps to lead to better financial performance and more importantly, improve the care of their member population.
Key Strategies for Optimizing Quality and Risk
In many provider organizations, quality and risk are handled by different departments leading to duplicative efforts and silos of information. Coordinated efforts that improve quality reporting and optimizing RAF scores will have a more substantial positive effect on the success of an ACO than individual efforts. The two are not mutually exclusive.
To start, it is critical ACOs establish a culture that aligns with its goals – improve quality and lower costs to best support the population for which they are responsible. This must be a top-down initiative that holds leadership, clinicians, and staff accountable for achieving quality and cost goals.
An ACO’s culture needs to be inclusive and collaborative by engaging physicians and other frontline providers to increase their buy-in while integrating practice improvement into their daily workflows. They must be part of the solution from the outset. By including these key team members from the beginning, you will understand what works best and how to design it, and the entire ACO team will take on a vested interest in making it successful. They become your champions reaching for the Triple Aim.
Establishing an interdisciplinary workgroup with representation from the Accountable Care Organization leadership, clinicians, clinic managers, operations, and coding will lead to improving the accuracy of documentation. Afterall, documentation is the foundation for quality reporting and HCC coding which determines RAF scores.
The workgroup can ensure that:
1) There is a complete and accurate problem list for each patient. This must be updated each year, with all diagnoses properly documented. Supporting data can be found in Electronic Medical Records across the organization and other treatment locations.
2) Patients are seen each calendar year. It is vital to see those patients who have chronic conditions annually to monitor, treat, and educate them on their conditions with the intent to prevent costly hospital stays. Annual wellness visits can also enable a provider to address many of the quality measures that are required.
3) Retrospective, prospective and concurrent chart reviews are conducted. Retrospective reviews will identify gaps in care and enable the team to work to close these gaps. Resubmitting claims where information was missed will offer the opportunity to enhance your current financial position. Prospective reviews will arm providers with information prior to a patient arriving. This will make it easier for a physician to discuss potential conditions with their patients. Concurrent reviews, medical notes and HHC codes are reviewed prior to claims submission, ensuring documentation supports the reported diagnoses.
4) A Clinical Document Improvement program is implemented. Educating providers about the importance of accurately documenting patient conditions promotes better care for their patients and assists in the financial well-being of the ACO.
In order to monitor performance in addition to managing patient population and financial risk, it is essential to have a strong analytics platform that shares data from within the organization and from the entire network of providers who support its beneficiaries. Without data analytics, an ACO is not able to accurately forecast costs, and outcomes will be compromised. Just having data is not enough. The ACO needs to leverage Electronic Health Records and Population Health tools that are integrated at the patient level and within provider workflows that make the data actionable at the point of care.
Finally, ACOs must improve transitions of care. Being responsible for the total costs of care for their population, ACOs want to ensure their members get the right care, at the right time, at the right location. By establishing a network of high-quality, low-cost, post-acute providers, ACOs can see lower length of stays and lower readmission rates.
As we continue down the path of alternative payment models, Accountable Care Organizations can be successful at generating cost savings (aka, lowering costs) and improving the quality of care for their members. Successful ACOs are creating a culture of collaboration, taking a holistic view of the population, leveraging data analytics, and ensuring access to the right care at the right time for the beneficiaries. Achieving these while arming providers with knowledge will lead to the outcomes we all desire – higher quality of care at lower costs.
Vee Healthtek, a leading global, technology-enabled professional services organization, is helping many accountable care organizations create a collaborative culture, identify gaps in care, and educate their providers to support these outcomes. These initiatives are yielding impressive results with our clients who are now closer to achieving the Triple Aim.
Donald M. Berwick, MD, MPP, President Emeritus and Senior Fellow, Institute for Healthcare Improvement. (2020). Triple Aim – The Best Care for the Whole Population at the Lowest Cost.

