A large hospital system from the east coast was concerned about poor documentation and its effect on their RAF (Risk Adjustment Factor). The data for the hospital system’s geographical location indicated a sick patient population of 44%, however, their hospital system data recorded the sick patient population at 35%
The hospital approached Vee Healthtek with these concerns. The General Manager of Coding at Vee Healthtek suggested a plan that included a retrospective sample audit for all physicians for a given period. As part of the review, Vee Healthtek would capture the current risk scores based on the claims submitted, and upon reviewing the medical records, would suggest updated risk scores. Additionally, Vee Healthtek would capture clinical documentation improvements by providers and clinics.
The Hierarchical Chronic Condition (HCC), also known as Risk Adjustment coding, is designed to access future healthcare costs of patient populations by assigning risk scores based on the diagnosis. HCC helps hospitals better understand sick patient populations to plan/provide the best care for patients. The accuracy of documentation and corresponding codes captured are critical to determining the exact risk condition with the highest specificity. The Risk Adjustment Processing System (RAPS) and Encounter Data Processing System (EDPS) are currently accepted by most payers to assess risk populations, and accordingly, allocate money for patient care. However, this will transition exclusively to EDPS by 2020, making the accuracy of documentation even more critical at the encounter level.
The accuracy of documentation also helps with:
-
Better Patient Care. Accurate documentation and capturing appropriate risk scores helps to improve patient treatment.
-
Increasing Revenue. Higher risk scores yield better revenue for physicians and hospitals. Providers spend most of their time with patients and prefer to minimize documentation time. They tend to use a standardized template or select more generic codes that do not necessarily yield the highest risk score for a given patient’s condition. Accurate documentation and correct corresponding codes result in increased reimbursement, and timely adjudication of claims, by the payers.
-
Maintaining Compliance. Compliance plays a significant role in the overall healthcare process, but primarily impacts documentation and coding. The accuracy of documentation and coding according to guidelines and standards helps hospitals improve their ratings.
-
Improved Care and Incentives. The MIPS (Merit-Based Incentive and Payment System) is calculated based on the quality of documentation and patient care by physicians. Documentation accuracy helps earn a better reputation and ensures reimbursement to doctors.
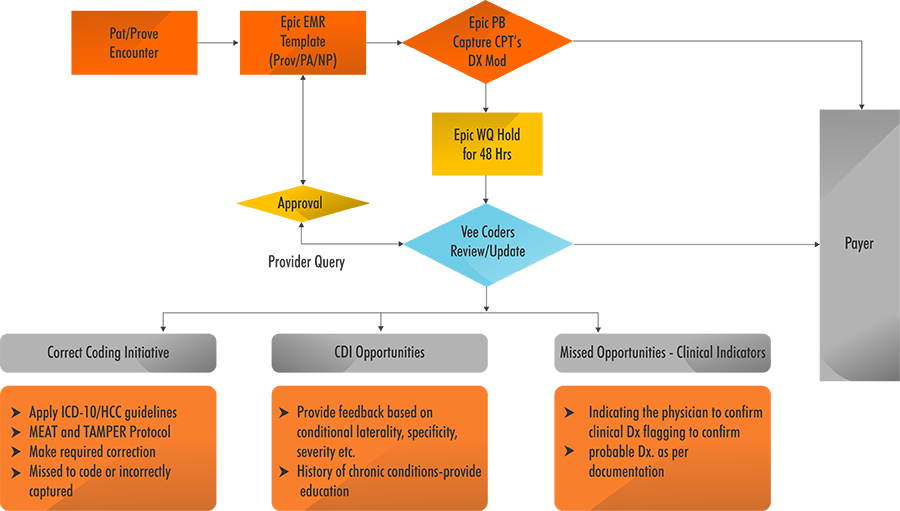
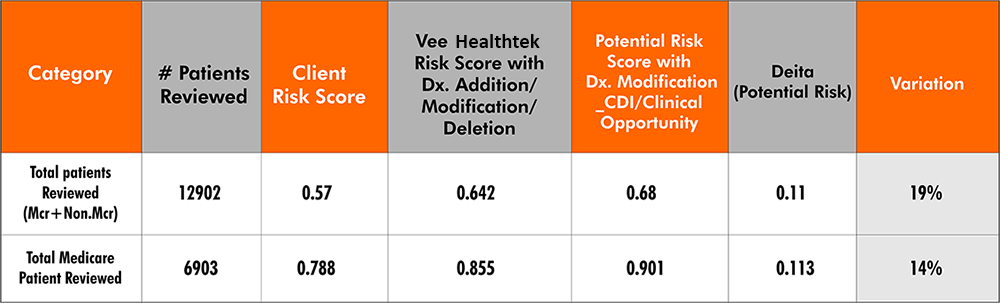
Vee Healthtek used the RADV audit standard and sample size for retrospective HCC review and the CDI program implemented for this hospital system. There were approximately 220 providers in the hospital system. Vee Healthtek reviewed 201 cases per provider for the given period of one year. Vee Healthtek deployed 30 HCC coders to work on the project with the goal to complete the review and finalize findings in 60 days to accommodate the client’s Fiscal Yearend. Vee Healthtek coders reviewed every case with the following focus:
- Correct Coding. Codes entered and billed were compared with the documentation of medical records for each encounter and for each prior visit in that calendar year. Discrepancies were captured to reveal the impact on risk scores and reimbursement.
- Identify CDI Opportunities. The cases were reviewed based on the severity, laterality, and specificity as per the current and previous visits documented for each patient. Opportunities with excluded documentation were chosen, which had the potential to improve documentation and increase risk scores for patients.
- Identify Missed Opportunities. Based on the clinical indicators, areas where risk adjusted diagnoses were not documented and reported but were actively treated by the provider were identified. This review also included identifying missed query opportunities (based on clinical indicators) to confirm any suspected missed opportunities.
Vee Healthtek reviewed over 35,000 cases for almost 13,000 patient accounts in eight weeks. The findings were presented showing the initial risk score, and the risk score identified based on corrected coding and missed documentation changes. For missed opportunity criteria, potential changes in the risk score were shown contingent on physician review and comments. Additionally, the detailed CDI (Clinical Documentation Improvement) report was created for each provider and clinic, identifying opportunities for education and improvement. Vee Healthtek suggested implementing a concurrent review of charts before billing to capture accurate risk scores to avoid lost revenue.
Accurate Risk Scores to Avoid Lost Revenue
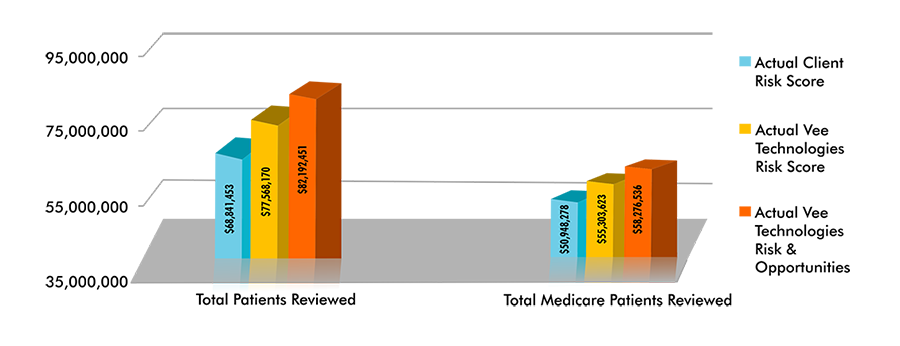
With this information, Vee Healthtek implemented a concurrent review of charts in order to capture accurate risk scores, improve reimbursement and create a provider education program through CDI opportunities. In doing so, it eliminated previous issues encountered and set the client up for success.